Experiencing pelvic organ prolapse can be challenging – it can interfere with your activities, intrude on your personal life, and be just plain uncomfortable.
Types and Causes of Pelvic Organ Prolapse
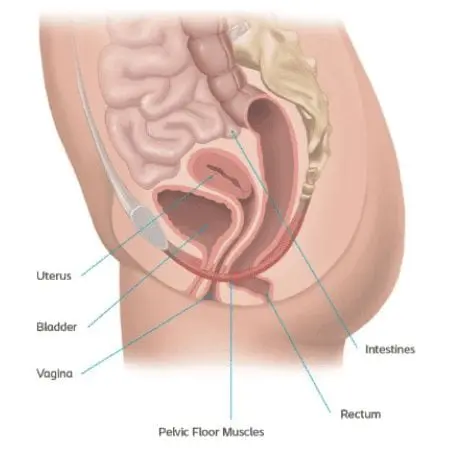
Pelvic organ prolapse (or POP) is a condition in which one or more organs in the pelvis descend due to a loss of support from the pelvic floor. The pelvic floor is a group of muscles that support the bladder, uterus, vagina, small bowel, and bowel. They are often described as being shaped like a hammock.
Normally these muscles and surrounding tissues keep the pelvic organs in place. Sometimes they can become too weak or stretched to continue supporting your pelvic organs. Organ shifting that happens because of these weak muscles can result in one or more types of prolapse.
To better understand the different types of prolapses, it is important to understand which organs have shifted as well as in which space of the pelvic floor became weak which results in different types of prolapse.
Front (anterior) Wall Prolapse
Bulging of the pelvic organ outside of the body is one possible symptom. Another symptom may be some form of urinary incontinence.

Cystocele Prolapse
Occurs when the bladder protrudes into the vagina due to the anterior (front) vaginal wall becoming weak.
Back (Posterior) Wall Prolapse
A bulging sensation is one possible symptom. Another symptom may be stressful bowel movements, either straining during bowel movements or not feeling like you evacuated all of your bowels. Lastly, you may experience the need to put your finger into your vagina or rectum to help fully empty your bowels.
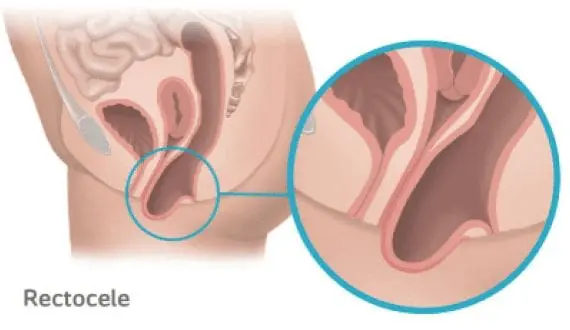
Rectocele Prolapse
Occurs when the rectum protrudes into the vagina due to the weakening of the supporting tissue.
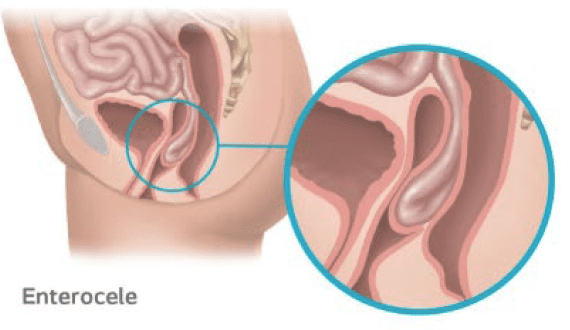
Enterocele Prolapse
Occurs when the small intestines protrude into the vagina due to the weakening of the support tissue.
Top of the Vagina
A bulge or feeling pressure are usually the most commonly found symptom.
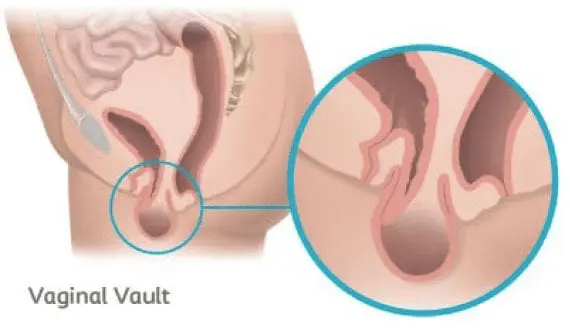
Vaginal Vault Prolapse
Occurs when the top part of the vaginal wall loses support and drops into the vagina.

Uterine prolapse
Occurs when the top part of the vaginal wall loses support and the uterus drops into the vagina.
Potential Causes of Prolapse
Pelvic organ prolapse is common. Over 3 million women in the United States suffer from Pelvic Organ Prolapse (POP). There are certain risk factors however which may increase your likelihood of experiencing prolapse.
Risk Factors Include:
- Vaginal childbirth
- Menopause
- Obesity
- Chronic cough
- Frequent constipation
- Pelvic organ tumors
Symptom Checker
Women experiencing prolapse won’t always experience obvious symptoms. As prolapse progresses, the symptoms may become more apparent and painful.
If you are experiencing prolapse, you may feel:
- Stress or pressure in the pelvic region
- Vaginal discomfort pain, pressure or bleeding
- Pulling or aching feeling in the lower abdomen or pelvis
- A bulge distended from the vagina
- Pain or uncomfortable sexual intercourse
- Difficulty urinating or having a bowel movement
If you are suffering from any of these symptoms, you may have prolapse and should consult with your doctor. Remember, although these signs and symptoms can alert you to a problem, they are not unique to prolapse, so it is important to consult a doctor for the correct diagnosis.
How is Pelvic Organ Prolapse Diagnosed?
Prolapse is a very common problem affecting millions of women. However, many women believe that their condition is a normal part of aging. Others are unaware of this condition and its treatment options. With the treatment options available today, women no longer have to live with this uncomfortable condition.
After discussing your medical history and symptoms with your physician, they should perform a pelvic exam, using a speculum, to confirm a diagnosis. You may need additional tests to determine the type of prolapse, the cause and the best treatment options for your condition.
Additional Exams May be Necessary
pelvic ultrasound
A diagnostic exam that allows your physician to view the organs and structures within your pelvis.
pelvic MRI
Provides images of the pelvic area to allow closer examination of your pelvic organs and structures.
urodynamic study or testing
Focuses on how the bladder, sphincters and urethra work together to store and release urine.
cystoscopy
Involves your physician using a cystoscope (rigid or flexible) to visually examine your bladder and urethra.
defecography
A radiologic study to look at bowel function and any prolapse symptoms that may be present.
What are the Treatment Options for Pelvic Organ Prolapse?
Don’t be discouraged by your condition. Half of all women between the ages of 50 and 79 say they have prolapse symptoms.1 There are different options you can consider to treat pelvic organ prolapse. Your treatment will depend on the type of prolapse you have as well as your future plans, which may include pregnancy.
It is important to understand your body and learn about all your treatment options, both non-surgical and surgical, to help find a solution that is right for you. Seek out a specialist who specializes in pelvic floor treatments and discuss your options to find the best solution for you.
Non-surgical Management Options
Prolapse may be managed with vaginal pessaries, Kegel exercises, biofeedback, and lifestyle changes. These options may involve long-term treatment, on-going maintenance, and continued expenses, and they may not address your underlying condition.
vaginal pessary
A device that’s placed in the vagina to support the pelvic floor and support the prolapsed organ. Your physician will fit and insert the pessary, which must be cleaned frequently and may have to be removed before intercourse.
kegels
Exercises that you can do on your own to help strengthen your pelvic floor muscles.
biofeedback therapy
Involves learning how to notice and working to control your body’s functions. While a monitoring device is placed by your physician, you will be asked to use your pubococcygeus muscle to see how much strength you need to contract your pelvic floor muscles correctly.
Surgical Management Options
Surgical repair can be done through the vagina or through the abdomen.
anterior or posterior colporrhaphy
The wall of the vagina is strengthened with sutures so that it once again supports the pelvic organs.
vaginally placed biologic tissue
Done through an incision in the vagina.
sacrocolpopexy and sacrohysteropexy
Done through the abdomen to repair vaginal vault prolapse and uterine prolapse with surgical mesh.
Reconstructive surgery of the pelvic floor is performed with the goal of restoring the organs to their original position. If you are considering surgery with the use of surgical mesh to repair your POP, ask your surgeon these questions before you agree to the procedure:
- Are you planning to use mesh in my surgery?
- Why do you think I am a good candidate for a prolapse repair procedure with mesh?
- Why is surgical mesh being chosen for my prolapse repair procedure?
- What are the pros and cons of using mesh in my particular case?
- Will my partner be able to feel the mesh during intercourse?
- Could my prolapse be repaired successfully without using surgical mesh?
Frequently Asked Questions
We’ve compiled some of the most common questions that men ask when learning about pelvic organ prolapse. Read for yourself to learn more about pelvic organ prolapse causes, symptoms and treatment options.
How common is Pelvic Organ prolapse?
It is estimated that approximately 3.3 million women in the United States suffer from pelvic organ prolapse.2 Pelvic organ prolapse is especially prevalent in women ages 50-79. About 50% of women in this age group indicate that they suffer from POP symptoms.3
What causes pelvic organ prolapse?
Pelvic organ prolapse can develop when events or activities happen that lead to increased pressure on the pelvic floor. Pregnancy and childbirth are often the most common cause of pelvic organ prolapse due to the increased stress placed on the pelvic floor muscles, but these are by no means the only causes. Genetics, lifestyle (smoking), chronic constipation, obesity, and many factors are connected to pelvic organ prolapse.
What are the symptoms of pelvic organ prolapse?
While some women do experience symptoms related to pelvic organ prolapse, many others may not notice any symptoms at all. It may also be difficult to identify prolapse symptoms as they often progress very slowly and you may not notice changes until they become extreme.
Symptoms will often depend on which type of prolapse you are experience and the specific organ that is dropping. Some common prolapse symptoms include pressure or fullness in the pelvic area, backaches, painful intercourse, urinary problems, and constipation.
Can pelvic organ prolapse be treated?
Yes, pelvic organ prolapse can be treated. There are many different treatment options available for pelvic organ prolapse. It is important to discuss your individual situation with a pelvic floor specialist who will discuss what options may be appropriate for your specific situation.
What are the treatment options for pelvic organ prolapse?
There are many different treatment options for pelvic organ prolapse that include both non-surgical and surgical treatments. Non-surgical treatment options include lifestyle and behavior changes, physical therapy or the use of a vaginal device (pessary). Depending on the severity of your pelvic organ prolapse symptoms and general health, it may be recommended to consider surgery. There are different types of pelvic organ prolapse surgeries, so it is important to discuss your options with your physician in detail to ensure that you find a treatment option that is right for you.
What is a prolapse repair procedure?
Pelvic repair surgeries aim to correct a prolapse by returning the “dropped” organ to its normal position and restoring your pelvic floor support. The procedure can either be performed through small incisions in the vagina or abdomen. While the thought of any surgery is scary, you are not alone. Get the facts about pelvic organ prolapse repair procedure here.
How long does it take to recover from a prolapse procedure?
Every patient’s recovery time is different. It is generally recommended that physical strain, sexual intercourse, and heavy lifting should be avoided for six weeks after surgery, but the patient may resume other normal activities after two weeks or at the surgeon’s discretion. Your doctor will provide specific details about your individual recovery process.
What are the risks associated with a prolapse procedure?
Every surgery carries some level of risk. Mesh reinforced prolapse repair may not be suitable for every patient, and a thorough discussion between you and your doctor will enable both of you to determine if this treatment is right for you. Ask your doctor for more information about potential risks and complications, as well as your specific surgery and situation.
How do I select the right physician to treat my prolapse?
Finding the right physician to treat your prolapse is a very important step in seeking treatment. Several types of specialists may treat prolapse; however, there are physicians within each specialty who specialize in certain conditions and treatment options. Taking time to do your research can make all the difference in the care you receive.
Will my insurance cover the prolapse procedure?
Most insurance plans, including Medicare, cover these procedures. Consult your insurance carrier to find out the specific criteria for coverage. The reimbursement specialist at your physician’s office may also be able to help you get answers.
